EMS rotation
The PGY1 EMS rotation is one week and focuses on exposure to prehospital patient care through ride-along shifts with our EMS agency partners including fire-based EMS, third service EMS, emergency dispatch centers, and time with EMS physicians and fellows. Residents will attend fellowship conference and complete self-directed learning.
The PGY2 EMS rotation is three weeks and focuses on exploring roles of EMS physicians and prehospital niches. Opportunities include but are not limited to field response with EMS physicians and fellows, mobile integrated healthcare, EMS academies, helicopter EMS, pediatric critical care transport team, tactical, Hazmat, event medicine, search and rescue, and quality improvement.
Interested applicants should contact:
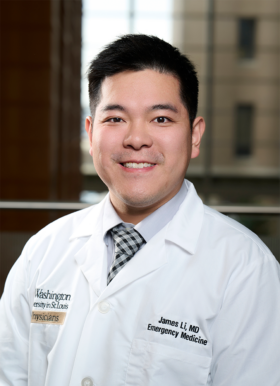
James Li, MD, MEd, FAEMS
Program Director, EMS Fellowship; Assistant Professor, Emergency Medicine
- Email: l.james@nospam.wustl.edu
Toxicology rotation
The toxicology rotation is a core component of emergency medicine residency education. PGY-2 EM residents rotate on the medical toxicology consult service for Barnes-Jewish Hospital and St. Louis Children’s Hospital. Residents evaluate and treat patients with acute overdose, unintentional toxic exposures, snake and spider envenomation, and critically ill poisoned patients. The goal of the rotation is to enable WashU EM graduates to independently care for toxicology patients in their future emergency medicine practices.
Rotation documents
- Directions to Toxicology suite
- Toxicology Essentials Rotation Guide (Residents, Fellows)
- Rotator Orientation
- Toxicology Core Curriculum 2021-2022
- After your rotation ends, please provide feedback on the Toxicology Rotation
Interested applicants should contact:
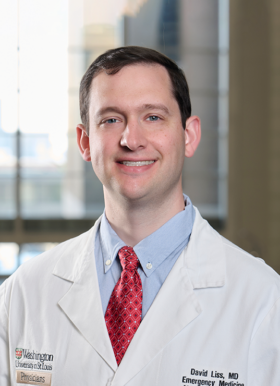
David Liss, MD
Division Chief for Medical Toxicology; Program Director, Medical Toxicology Fellowship; Associate Professor, Emergency Medicine
- Email: lissd@nospam.wustl.edu
Administrative support: Sara Delatte
Ultrasound rotation
This rotation will focus on emergency point of care ultrasound and all of its many applications and uses in the Emergency Department, including the FAST exam, pelvic ultrasound, Abdominal Aortic Aneurysm (AAA), cardiac, vascular access, renal, gallbladder, and DVT.
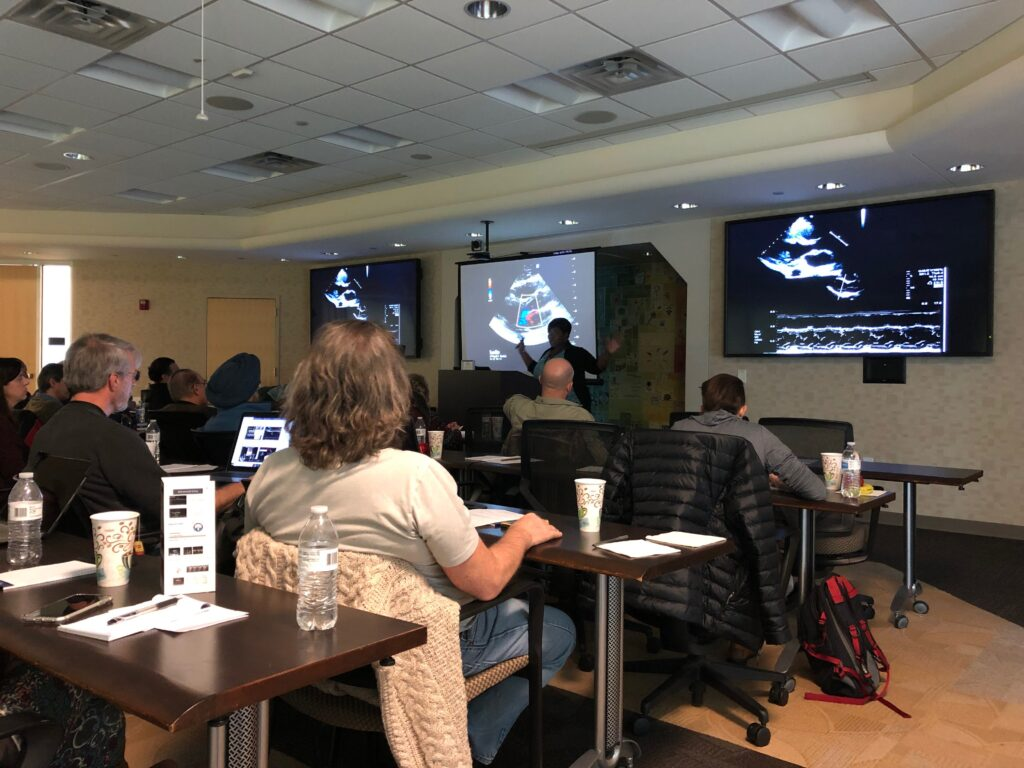
In general, the residents will be in the Emergency Department during weekdays to perform these exams. The ultrasound resident will serve as a consultant in obtaining clinically relevant ultrasound images and interpretation with oversight from the attending on shift and the designated ultrasound faculty member.
The ultrasound resident will record all ultrasound images into a storage archiving system that will be used to review images on a weekly basis during Quality Assurance. The ultrasound resident will also have weekly direct hands-on scan shift with the designated ultrasound faculty member. At the end of the rotation the student should have gained the knowledge of basic Emergency Ultrasound including it’s indications and applications; as well as becoming more adept at the performance of ultrasound. Learn more about the rotation on POCUS Hub.
Average number of patients seen each week: ~100 ultrasounds/week
On-call/weekend responsibility: none