Temperature Management Following Cardiac Arrest
Washington University Emergency Medicine Journal Club – August 19, 2021
Vignette:
You’re working a busy shift in TCC one Monday evening when you receive a page: “EMS to 6R with 65 yo male, cardiac arrest, defibX2 with ROSC, ETA 5.” You rush to TCC 6, assemble your team, and prepare your airway equipment. EMS arrives and reports that Mr. X is a 65-year-old male with a history of hypertension and coronary artery disease with previous stent placement 5 years prior. He was at home with his wife and teenage daughter when he suddenly slumped over on the couch and became unresponsive. While the wife called 911, the daughter felt for a pulse and began CPR when she could not detect one. EMS arrived approximate 10 minutes later and continued CPR while placing him on their monitor. They noted the following rhythm:
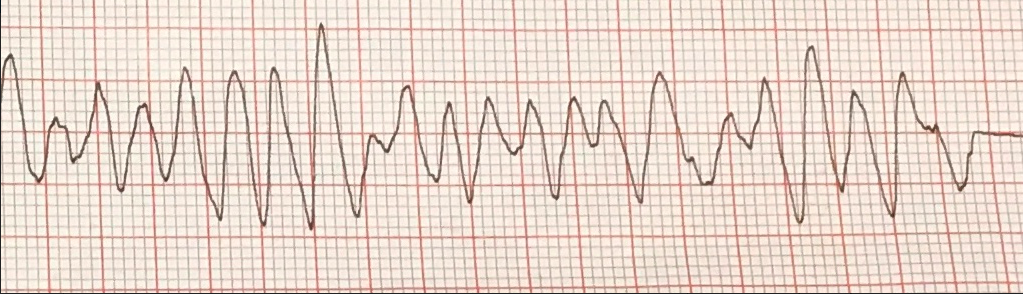
He was shocked twice, at 120 and then 150 joules, with return of spontaneous circulation (ROSC). At that time, an I-gel was placed and he was rapidly transported to the ED. He arrives with an I-gel in place, being bagged, with palpable femoral and carotid pulses. He remains unresponsive with fixed and dilated pupils. His initial blood pressure is 133/79 and his heart rate is in the high 80s. You are able to intubate him without RSI. His initial ECG reveals signs of left ventricular hypertrophy with a rate of 89, and is unchanged from prior ECGs in EPIC. His temperature, by bladder catheter measurement, is 36.8 degrees Celsius.
The nurse sends off the lab work and you confirm your ET tube placement with a chest x-ray. You place an admission order for the ICU and the critical care fellow calls back. After getting report, he suggests you consider placing a cooling line for induced hypothermia given the patient is post-cardiac arrest from ventricular fibrillation. You’ve heard of induced hypothermia before and remember reading that studies showed targeting a temperature of 36 degrees Celsius was just as beneficial as a temperature of 33 degrees Celsius. When discussing this with your attending, he tells you about a more recent study that found no benefit to induced hypothermia when compared with more conservative attempts to maintain normothermia. You forego the cooling line and send the patient to the ICU, but after your shift decide to take a deep dive into the literature to see what intervention is really most appropriate. On quick search of the journal club archives you find that this topic was covered in 2007, but you wonder what other evidence has come to light since then…
PICO Question
Population: Unresponsive adults following cardiac arrest with ROSC (return of spontaneous circulation)
Intervention: Induced hypothermia to 32-34°C
Comparison: Targeted temperature management to 36°C, induced hypothermia to 32-34°C , normothermia with early fever treatment, no cooling
Outcome: Mortality,neurological morbidity, post-arrest arrhythmias, other end organ viability/damage, cost-effectiveness, bleeding complications
Search Strategy:
PubMed was searched using the terms (induced hypothermia OR “targeted
temperature management“) and “cardiac arrest”, limited to clinical trials
(https://tinyurl.com/55wktk47). This resulted in 256 citations, from which 4 were
chosen
Article 1: Dankiewicz J, Cronberg T, Lilja G, Jakobsen JC, Levin H, Ullén S, Rylander C, Wise MP, Oddo M, Cariou A, Bělohlávek J, Hovdenes J, Saxena M, Kirkegaard H, Young PJ, Pelosi P, Storm C, Taccone FS, Joannidis M, Callaway C, Eastwood GM, Morgan MPG, Nordberg P, Erlinge D, Nichol AD, Chew MS, Hollenberg J, Thomas M, Bewley J, Sweet K, Grejs AM, Christensen S, Haenggi M, Levis A, Lundin A, Düring J, Schmidbauer S, Keeble TR, Karamasis GV, Schrag C, Faessler E, Smid O, Otáhal M, Maggiorini M, Wendel Garcia PD, Jaubert P, Cole JM, Solar M, Borgquist O, Leithner C, Abed-Maillard S, Navarra L, Annborn M, Undén J, Brunetti I, Awad A, McGuigan P, Bjørkholt Olsen R, Cassina T, Vignon P, Langeland H, Lange T, Friberg H, Nielsen N; TTM2 Trial Investigators. Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest. N Engl J Med. 2021 Jun 17;384(24):2283-2294. doi: 10.1056/NEJMoa2100591. PMID: 34133859. Answer Key
Article 2: Bray JE, Stub D, Bloom JE, Segan L, Mitra B, Smith K, Finn J, Bernard S. Changing target temperature from 33°C to 36°C in the ICU management of out-of-hospital cardiac arrest: A before and after study. Resuscitation. 2017 Apr;113:39-43. doi: 10.1016/j.resuscitation.2017.01.016. Epub 2017 Jan 31. PMID: 28159575. Answer Key
Article 3: Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Åneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Køber L, Langørgen J, Lilja G, Møller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H; TTM Trial Investigators. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206. doi: 10.1056/NEJMoa1310519. Epub 2013 Nov 17. PMID: 24237006. Answer Key
Article 4: Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002 Feb 21;346(8):549-56. doi: 10.1056/NEJMoa012689. Erratum in: N Engl J Med 2002 May 30;346(22):1756. PMID: 11856793. Answer Key
Bottom Line:
Multiple guidelines, including those from the American Heart association and the European Resuscitation Council, currently recommend targeted temperature management for patients with return of spontaneous circulation (ROSC) following cardiac arrest. Initial studies evaluated the utility of induced hypothermia, with temperature goals in the 32 to 34°C range. One of the more widely cited of these (Hypothermia after Cardiac Arrest Study Group, 2002) found a substantial increase in rates of favorable neurologic outcome with the use of hypothermia in this range following witnessed cardiac arrest with ventricular fibrillation (VF) or nonperfusing ventricular tachycardia (VT) as the initial rhythm (RR 1.40, 95% CI 1.08 to 1.81). The number needed to treat (NNT) for this intervention was 6. One primary limitation to this study was that a substantial number of patients in the “normothermia” group actually spent a significant amount of time with temperatures above 38°C. Previous research has demonstrated an association between hyperthermia and adverse outcomes following cardiac arrest (Zeiner 2001), and it is possible that the improved outcomes seen with induced hypothermia were simply due to avoidance of hyperthermia.
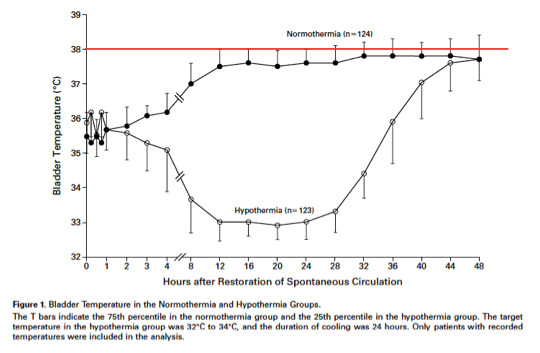
Partly due to this concern, later studies evaluated a more moderate hypothermia goal of 36°C, termed “Targeted Temperature Management.” The TTM Trial, published in 2013, compared a targeted temperature of 33° C or 36° C among patients admitted to the hospital following out-of-hospital cardiac arrest (OHCA) with any initial rhythm. There was no difference in all-cause mortality up to 180 days following enrollment (hazard ratio [HR] 1.06, 95% CI 0.89-1.28) or functional outcomes in the same timeframe. This and similar studies resulted in ILCOR and the European Resuscitaiton council updating their guidelines in 2015 with the less strict recommendation that a temperature of 32°C to 36°C be maintained in these patients.
Unfortunately, the real world application of more moderate temperature goals can lead to decreased compliance and increased adverse outcomes. This was demonstrated in a before-and-after study from Alfred Hospital in Melbourne, Australia (Bray 2017). After changing the targeted temperature for post-ventricular fibrillation cardiac arrest patients from 33°C to 36°C, the authors found a statistically nonsignificant trend toward decreased survival to ICU and hospital discharge as well as a trend toward decreased survival with a CPC score of 1-2. These trends toward worse outcomes were likely due to poor compliance during the 36°C phase, when nearly 1 in 5 patients had at least one documented temperature ≥38.0° C. Patients in the 33° C phase were also much more likely to receive pre-hospital and ED cooling than during the 36° C phase.
Given increasing evidence that prevention of hyperthermia, rather than induced hypothermia to a predefined goal temperature, improves outcomes following cardiac arrest, the international TTM2 Trial was conducted and published earlier this year. These investigators compared induced hypothermia to a temperature of 33° C with strict maintenance of temperature at 37.5° C or less. Hyperthermia was avoided in this latter group with surface or intravascular cooling devices. Patients in the two groups had similar 6-month mortality (RR 1.04, 95% CI 0.94 to 1.14), functional outcomes, and quality of life.
There is mounting to data to support the prevention of hyperthermia in patients with ROSC following cardiac arrest rather than universally inducing hypothermia. Given the potentially high cost and manpower required to place intravascular cooling catheters and apply surface cooling devices in these patients, a more conservative approach certainly has its advantages. The most recent TTM2 study demonstrates that not only is hyperthermia prevention achievable, but results in similar outcomes to induced hypothermia. Give the demonstrated issues with compliance in real-world application, care will need to be taken to maintain vigilance in these patients to prevent the harm associated with hyperthermia in the post-cardiac arrest period.