Burn Management in the ED
Washington University Emergency Medicine Journal Club- November 2020
Vingnette:
You’re evaluating a young male in the department for burns. Patient states that he
had a little too much fun last night and was wrestling with his fraternity brother too
close to the bon<ire, resulting in his left arm burn. The event occurred about 6 hours
ago, and the patient was concerned when he noticed the blisters this morning. His
primary exam leaves you with no concerns for other trauma or impending airway
doom. His left arm has a roughly 5% body surface area burn of a superficial partial
thickness burn, which is thankfully not circumferential. His arm is neurovascularly
intact distally and he notes his tetanus is up to date. Other than this “bro” being an
Alabama fan, and a lover of cheap beer, you have nothing else to work-up. He asks if
he is going to have a “graft” done like on the TV shows and if he will need special
medications for the wound. Suddenly, his Delta Delta (ΔΔ) sorority girlfriend enters
the room with a bedazzled mask, likely made of Swarovski crystals. She informs you
she is an “insta” model and cannot (CANNOT!) have her beau with any disfiguring
appearance – she inquires if essential oils and healing crystals may be of use. You
kindly excuse yourself to consult the horoscopes, but really it is to question if (1) the
area needs debridement or (2) other wound management, such as silver
sulfadiazine.
PICO Question #1:
Population: Patients with super<icial partial thickness burns (i.e. blistering burn),
BSA of 15% or less not involving areas that would require transfer to a burn center
(i.e. mucus membranes/upper airway, perineum, etc.) presenting to the Emergency
Department within 24 hours of thermal burn who are stable for discharge
Intervention: Debridement +/- topical wound care
Comparison: No debridement +/- topical wound care
Outcome: Wound appearance (healing) at 6-months, infection within 2-weeks,
procedural pain, pain control over duration of wound healing, ED length of stay
(many debridements require procedural sedation).
PICO Question #2
Population: Thermal partial thickness burns presenting to the emergency
department, who are stable for discharge
Intervention: Topical agents (antimicrobials, silver sulfadiazine, honey)
Comparison: No topical agent
Outcome: Wound infection, healing time, pain with changing of dressings, patient
satisfaction with wound appearance, cost, adverse medication effects
Search Strategy
No formal search strategy was employed.
Article 1: Swain AH, Azadian BS, Wakeley CJ, Shakespeare PG. Management of
blisters in minor burns. Br Med J (Clin Res Ed). 1987;295(6591):181. Answer Key.
Article 2: Gimbel NS, Kapetansky DI, Weissman F, Pinkus HK. A study of
epithelization in blistered burns. AMA Arch Surg. 1957;74(5):800-803. Answer Key.
Article 3: Ro HS, Shin JY, Sabbagh MD, Roh SG, Chang SC, Lee NH. Effectiveness of
aspiration or deroo<ing for blister management in patients with burns: A
prospective randomized controlled trial. Medicine (Baltimore). 2018;97(17):e0563.
Answer Key.
Article 4: Norman G, Christie J, Liu Z, et al. Antiseptics for burns. Cochrane Database
Syst Rev. 2017;7(7):CD011821. Answer Key.
Bottom Line:
In the United States (U.S.) over 1 million burn injuries occur annually, resulting in 486,000 emergency department (ED) visits, 40,000 hospital admissions, and 3275 deaths each year. While over 60% of burn-related hospital admissions occur at 128 burn centers, the other 4,500 U.S. hospitals average less than three burn admissions per year. However, most burns are superficial and minor involving <5% of the total body surface area and can present to any ED, so understanding basic management principles and the underlying clinical science is essential.
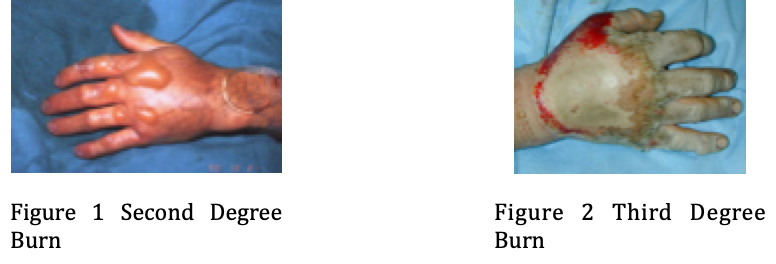
Burns can be secondary to heat, electricity, or chemicals. First-degree burns only involve the epidermal layer. They cause pain and erythema, but generally heal within several days without any scarring. Second-degree burns involve the entire epidermis and part of the underlying dermis. These burns are sub-classified into partial-thickness or deep partial-thickness burns. Partial-thickness burns appear as erythema with blister formation and weeping (Figure 1). They are exquisitely painful and blanch to pressure, which indicates preservation of the dermal circulation. Deep partial-thickness burns involve the entire reticular and papillary layers of the dermis and appear as a non-elastic red or white layer on top of the burn that usually does not blanch. These burns require up to three weeks to heal and can be associated with significant scarring. Deep partial-thickness burns are generally not sensitive, involve the entire epidermis and dermis, and can appear white or tan with a leathery texture (Figure 2). Deep partial-thickness burns often require surgical excision and skin grafts because they do not heal.
Burns can result in irreversible tissue necrosis at the center of the burn with the extent of injury dependent on the temperature (or concentration) of exposure, duration of exposure, and vascular supply. Blisters form when the dermis and epidermis separate with concomitant activation of the clotting and complement systems causing recruitment of inflammatory cells that release inflammatory mediators that increase vascular permeability with transudation of fluid and protein into the interstitial space. Blister fluid is complex: on one hand, fibroblasts and keratinocytes promote wound healing (Kupper 1986, Chen 1992, Wilson 1994); on the other hand, vasoactive prostanoids may increase secondary tissue damage by reducing microcirculatory flow. Blister fluid may also impede fibrinolysis and inhibit opsonic activity against Pseudomonas aeruginosa creating progressive dermal necrosis (Deitch 1985, Rockwell 1989).
A minor burn involves less 5% total body surface area. Circumferential burns, as well as those involving the face, ears, eyes, perineum, joints, or in those with renal failure or diabetes, are not considered minor burns. Physicians often disagree when estimating the size and severity of burn injuries (Hammond 1987, Wachtel 2000) In addition, for partial thickness burns there are no well-accepted guidelines or standard of care for initial management. In fact, management guidelines sometimes contradict one another and have for nearly a century (Cope 1943, Lewis 1954, Wallace 1951). For example, whereas Singer et al. suggest leaving small burn blisters intact, Allorto et al. note that “removal of all blisters facilitates accurate assessment of the burn size and depth”. Experimental animal models imply that removing the necrotic epidermis delayed re-epithelialization, increased infections, and led to worse scarring. Decades old studies by Winter, Hinman, and Wheeler demonstrated that a moist wound environment (which intact blisters create) benefits wound healing.
Wound healing, infection rates, discomfort, and financial cost should be the highest priority outcomes. When considering specific interventions, such as debridement, pragmatic healthcare teams also need to specifically consider ED length of stay, pain control, and the potential costs and unintended consequences of procedural sedation. Unfortunately, there is currently a paucity of literature regarding these specific topics with very little evidence comparing in-ED (i.e. blister aspiration, deroofing, debridement, or leaving blisters intact) or post-ED (topical agent) management options. We evaluated the highest quality published research on these topics for our deep-dive journal club analysis on this topic.
Ro, et al. (2018) compared aspiration and deroofing of thermal blisters in a randomized, controlled fashion. Patients’ perspectives of burn pain and overall healing appearance differ from that of the physicians. Patients allocated to the deroofing group reported increased pain and concern for disfigurement compared to the aspiration group. This study highlights the importance of patient perception of recovery when initiating burn care. Additionally, this study found a trend toward decreased bacterial colonization in the aspiration group when compared to the deroofing group, but did not assess for clinically relevant infection (e.g. cellulitis), an important outcome for both the patient and the provider.
Swain et al. (1987) compared outcomes in small blisters that were either left intact, aspirated, or deroofed, looking at patient experience with pain and bacterial colonization. Patients who had deroofed blisters reported more pain compared to the other groups. Intact blisters also conferred the lowest rates of bacterial colonization. Unfortunately, this was an unblinded study and its reporting methods were unclear, which severely muddied data interpretation.
Gimbel et al. (1957) provided us a blast from the archaic past, where medical students “volunteered” to receive thermal-induced controlled burns with blisters. The histology of the burns and overall healing were evaluated at specific times after the initial injury. This study offered no control group and no blinding. However, the results revealed that intact blisters healed faster compared to those either aspirated or deroofed. They did not assess burn pain or cosmetic appearance and did not evaluate for wound infection. Most minor burn blisters resolved spontaneously within 12-days as atmospheric water loss exceeded dermal fluid diffusion as epithelium regenerated between the healing dermis and epidermis. This 63-year-old study provides histological evidence of epidermal healing and hypothesis-generating proof that neither aspiration nor unroofing of burn blisters is preferred to leaving the blister intact.
Finally, an extensive Cochrane review by Norman et al (2017) evaluated antiseptics and antibacterial interventions for burn wounds. The authors found high risks of bias in the majority of the studies reviewed, yielding a low to moderate certainty of evidence. They did include GRADE scores, a systematic approach to evaluating evidence in systematic reviews and other bodies of literature. Much can be gleaned from this work, including evaluation of potato peels and amniotic membrane for burn wound care, but the big question revolves around the reigning champion, silver sulfadiazine. Silver-containing dressings were found to be just as effective as silver sulfadiazine for wound healin, and may allow wounds to recover faster. Honey was also evaluated, and was found to be a fantastic option for burn wound management as well! Some studies found that honey was more effective than silver sulfadiazine in assisting with wound healing and with quick recovery times.
Bottom Line: Looking forward, a prospective study comparing conservative management, aspiration, and deroofing of thermal blisters in a randomized, double-blinded study with patient-centric outcomes would offer more conclusive results. Unfortunately, although trials of expensive biomedical alternatives to skin grafts like ReCell are underway, no known trials addressing the simple question of deroofing exist on ClinicalTrials.gov at this time. Shaw and Dibble (2006) and Singer (2007) (emergency physicians) both recommend leaving thermal-induced blisters intact based on studies demonstrating favorable outcomes (decreased pain, faster wound healing, lower bacterial colonization) and our critical appraisal of published research supports that recommendation. For partial thickness burns involving small body surface area, leaving blisters intact is a reasonable treatment option. As for antiseptics, honey has surprising efficacy at preventing wound infection! While many hospitals may not currently carry honey in their pharmacy, most are likely to have well-stocked cafeterias. Alternatively, silver sulfadiazine has withstood the test of time and is a viable option, and silver-containing coverings have demonstrated similar antibacterial effects and wound healing benefits.